
That healthcare is expensive is widely known. So, citizens should accept health services with gratitude and respect.
But looking at healthcare delivery model as a citizen and a patient (not as a professional healthcare administrator), one can spot at least three areas where money could be saved for the benefit of patients.
Avoidable hospitalizations.
General practitioners (GPs) are overloaded almost everywhere. As a result, patients are often too easily pushed to hospitals instead of being treated in the comfort of their homes.
A typical story: a man in Germany was experiencing a severe cough, dizziness, fever and breathlessness. Such symptoms can indicate a flue, bronchitis, but also sometimes heart failure up to the upcoming infarction. A local GP who appeared only the next day suggested an immediate hospitalization. Already surviving the night, a patient was apparently not keen on the perspective. ”Why to go to the hospital right now?” “Because – replied a doctor with authority – you have already had a history of heart problems. Besides I don’t understand why you don’t want to go to the hospital”. A surprise was so genuine as if she was proposing to drop into a nearby pub.
True, the sick person went through heart operation with several bypasses about 10 years ago. But is that a sufficient reason to drag him to the hospital exactly at the moment? Fortunately, this man urgently demanded the troponin blood analysis (protein found in heart muscle that are released into the blood in case of the heart damage) to rule out myocardial infarction. On top, he requested the ECG. Both analyses can be performed at home. The result on the troponin was negative. There was no urgent need for a hospitalization.
This case is not unique: according to the World Health Organization (WHO), 20% of hospitalizations in Germany in 2012 were preventable or totally unnecessary: in other words, the hospitalization of every fifth patient could have been avoided through timely and effective provision of ambulatory care.
The outcome of the story this time was positive. Another GP came diagnosing bronchitis and allowing the man to stay at home. It took about 20 euros to pay for the medications vs. thousands that could have been spent to cover a few days in a hospital. It was also a human factor that made the difference: the physician with the ambition to help his patient. The system was obviously prioritizing hospitalization over the ambulance care.
Bureaucracy vs. care.

No doubt healthcare is a very complex business. It is proved by numerous medical protocols guiding medical procedures. “Primum non nocere” or “first, do no harm” is a fundamental bioethical principle every medical student is taught at school. It is better to do nothing, than to risk causing more harm than good to your patients.
However, blunt adherence to prescribed rules can cover professional incompetence and indifference.
Another typical story: a man in his early sixties, strong and sporty, suddenly felt dizzy. He diagnosed himself with the approaching stroke. Knowing that there is a window of three hours within which help should be delivered, he called the ambulance. Within those 3 hours a neurologist should perform a brain computer tomography (CT) to determine the nature of stroke. In case of ischemic (which is over 80% of all strokes), some of the blood vessels are blocked by a thrombus (fat or blood clot) that disrupts the blood flow from reaching certain areas of the brain to supply it with oxygen. The thrombolytic drugs can dissolve the clots, reestablishing the oxygen supply. The same treatment, however, can kill when a weakened blood vessel ruptures spilling out the blood into the brain. The so-called hemorrhagic stroke.
The arriving emergency took a man to the nearby hospital in the city of Freising (in Bavaria, Germany). Unfortunately, it was Sunday night. Worst time getting to the hospital as all specialists are fast asleep expected to be back the next morning. The assistant doctor on call this night was not an expert in reading CT brain images, nor was she allowed to. Only a trained neurologist can read the CT image to detect lesions in patients. So, the decision was simple: wait for the next shift of neurologists to come leaving this patient for 6 hours without any help in the emergency department.
Unfortunately, the stroke was not aware of such human constraints. It let itself develop. The patient in question was sitting meaninglessly before the assistant doctor on duty who diligently filled the lengthy protocol. “Better to do nothing” condemned this patient, who came to the hospital only with minor impediments, to years of paresis.
Should this doctor dare to wake up a neurologist, a man would have received a proper treatment, e.g., with thrombolytic medications, anticoagulants, antiplatelet agents, for instance, a simple heparin injection, as well as antihypertensives and peacefully returned home after spending a couple of days in a clinic. In extreme case, an endovascular device could be applied. The whole procedure would have probably cost several hundred euros. But alerting a colleague in the middle of the night was not mentioned in medical guidance. The logic of the caregiver that night was unassailable: nothing personal, I am doing my job according to instructions.
Recently I have learned that the Freising hospital had made an agreement with the large University clinic in Munich. Professional neurologists can now provide 24×7 remote video consultancy and in extreme cases personally come to Freising. I assume that the above described case was not unique, and the accumulation of similar cases eventually outraged both patients and authorities. But how many lives should be disturbed before the decision was taken?
Avoidable surgeries or cunning economics.

Too often medical professionals resort to radical interventions without sufficient reasons. Money is lavishly spent on medical procedures, which are not only needless, but may be harmful.
Thus, according to AOK 2014 report (AOK is one of the largest German health Insurance houses): 19,000 deaths could be prevented, should unnecessary surgeries be avoided.
For a comparison: car accidents in Germany took away the same year 3.290 lives. The situation in the US seems to be no better. Avoidable surgeries might account for 10% to 20% of all operations in some specialties, including a wide range of cardiac procedures. According to the Medical Experts Online, the US company that provides patients a platform for a second medical opinion, in 66% of cases the first recommendation in favor of surgical intervention was found inappropriate.
Studies revealed that physicians were often “incentivized to perform surgical procedures, either for financial gain, renown, or both”. Many of them complained “surgery quota” was imposed on them by health administrators, due to the provisions hospital were getting from insurances for each operation. Considering that a surgery costs on average about 40K – 50K euro, the business seems lucrative.
James Rickert , MD, an orthopedic surgeon in Bedford, Indiana thinks that hospitals recommend patients to undergo surgery“ because they are paid approximately ten times more money to perform surgery than to manage one’s problem conservatively.
It is not accidentally that the modern healthcare system was traditionally focused on treating the disease vs. preventing it and supporting health. As one cardiologist with 19 years of experience formulated: “The key is that the early prevention won’t make profit. In treatment, operations like placing stent will be profitable, while oral education on prevention won’t make great financial benefit. Patients spend a lot when they get diseases”.
Perhaps such economics is good for insurances and some hospitals, but effectively it is just a money wasting: it is a patient who ultimately pays with both his money and health.
Professional health managers and scholars can provide deeper analysis on healthcare economy, but from a patient perspective the healthcare system we currently have is rather optimized for generating revenue than for the effective care. Paradoxically, in this way the system is losing both: money and efficiency.

Imagine: suddenly you feel dizzy. You simply press the button of your smart band, watch, necklace, etc. Your ECG, glucose level or blood pressure will be immediately checked, and Artificial Intelligence (AI) software will recommend simply to sip 20 mg of Cognac and peacefully go to bed. Would it be nicer than calling the emergency?
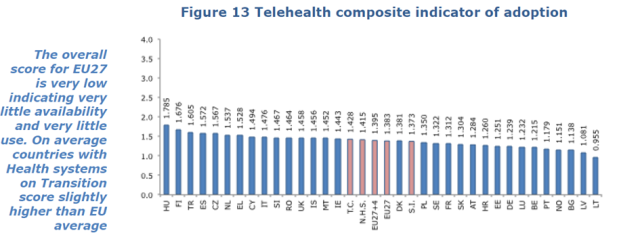
Indeed, promises of the 3d Digital Wave are breathtaking. With 70 percent of healthcare organizations worldwide investing in consumer-facing technologies, e.g., wearable sensors and related apps, patients are expected to receive virtual medical care anytime anywhere. Artificial Intelligence will compensate the lack of a human one. It will disrupt the existing healthcare system by delivering easily accessible, cheaper and higher quality care to 70% of patients by 2025. Researchers at Stanford University have recently compared 130,000 images of 2,000 different skin lesions into a computerized algorithm discovering that artificial intelligence was just as good as 21 board-certified dermatologists at identifying instances of skin cancer. By 2020, cognitive systems are expected to diagnose in minutes such chronic conditions as cancer and diabetes. 75% of all patients hope to witness such glorious metamorphosis.
According to the studies the second wave of digital health transformation has already provided European citizens with electronic health records (EHR), particularly in Germany.
As a patient, I wonder: where are all those treasures? Who is hiding them from me and other patients, and where? Entering a nearby hospital (by the way, in modern Germany) I have a feeling that those is who are writing futuristic those visions live somewhere in a different world, not in the one most of us, ordinary citizens temporarily grieve in. For sure, EHR has already been implemented somewhere, but as I was searching for an X-ray image buried in one of the hospital’s archive departments (not to be confused with Picture Archiving and Communication System/ PACS) I was, with many difficulties, provided with a printed film. An image depicted a spinal injury with no trace of a cardio operation that was, according to the records, performed upon the patient a week ago. Moreover, it was obvious that an image belonged to a woman, while the patient we were concerned about was unquestionably a male. The authentic image, by the way, was never found.

Meanwhile, some of the technologies able to help millions in diagnostics and treatments have already existed for years. For example, the Canadian company Biosig Instruments has patented the InstaPulse® Heart Monitor that registers arrhythmias without the use of common 12-lead medical devices available only in hospitals, cardiology clinics and, sometimes, in advanced physicians’ offices. One can simply grasp the device with both hands and it will automatically turn on continuously updating your cardio rhythm. Note that irregular cardio rhythms are causing the formation of blood clots in vessels. The blockage of the vessel depending on the location can provoke congestive heart failure, ischemic attack or even myocardial infarction (with necrosis) and stroke. Though the device was registered as a “fitness gadget” (apparently to avoid the FDA hassle) it could be well applicable to cardio patients. Cardiological Clinic Aachen in Germany is now using almost identical device to treat their stroke patients.

The Insta-Pulse® Heart Rate Monitor was invented by Dr. Gregory Lekhtman for a general consumer in 1975 being sold for 128 Canadian dollars. Researchers in Aachen started experimenting with their device in 2016. The calculated distance (airline) between Germany and Canada is approximately 6,750 Kilometer. About 1000 hours walking distance (given the ocean were replaced by the firm ground). It took almost 50 years for physicians to start practicing comparable device in Europe.

Similar fate apparently befalls wearable garments such as Niturit, a seemingly ordinary T-shirt developed by the University of Aveiro in Portugal and the Israeli “Moked Enosh” company. The sensor enabled garment records ECG signals transmitting the results via a smart phone over a number of days directly from a patient to a cardiologist. The T-shirt was offered years ago as part of examinations by the Moked Enosh center at the cost of $ 117. While the European Space Agency was quick to choose this T-shirt to test astronauts, cardio patients are still awaiting it in their nearby hospitals.
No question, there are oases of innovations such as Mayo or Cleveland Clinics, or Kaiser Permanente being on top of the technological edge. Yet patients are less concerned about “best practices”, but rather with the “broader adoption” of innovative methods as part of a routine healthcare procedures.
We consume digital services daily in highly competitive and consumer oriented industries such as banking, manufacturing or retail. But healthcare still remains most highly impenetrable fortress for IT innovations. Just as we see disconnections of IT systems in many of the hospitals, so we observe a disruption of knowledge flows within the medical community. Such methods as “crowd funding” or “crowed testing” so familiar, e.g., in software development practices are not yet widely spread in healthcare environment.
Why the technologies that can make our healthcare more efficient, personalized and accessible are slow to reach the consumers?
To justify the inborn conservatism, medical professionals often refer to the fundamental bioethical principle of “Primum non nocere” or “first, do no harm” every medical student is taught at school. It is better to do nothing, than to risk causing more harm than good to your patients. Of course, healthcare has to deal with subjects much more complex and multifaceted than, e.g., manufacturing or finance. But if Niturit or HealthWatch, 15-lead ECG-sensing T-shirt that can read heart rate, blood pressure, detecting cardiac irregularities, have already been tested on a number of patients including astronauts, why other hospitals at least do not check on them? Are astronauts much more important than the rest of us citizens?
True, new delivery models will demand changes in traditional health bureaucracy and administration. How to combine, e.g., remote consultancy with the traditional face-to-face visits? Who will actually be responsible for the remote monitoring? How those remote services will be compensated by insurances? However complicated all those challenges may seem, solutions can be found. Other industries have coped with those problems rather quickly. Banks have adjusted their administration and personal issues to online payments and even software industries moved rather quickly from licenses to pay for services model.
Maybe the reason for delays is that there are simply too many of us patients around the world, so healthcare organizations have relatively low competition pressure compared to other industries? With population growing older and over 44% of World Health Organization Member States to have less than 1 physician per 1000 population patient, medical providers will hardly be left without jobs. Unlike other industries forced to fight for their customers by offering them better services, the problem in healthcare is reverse: how to reduce the patients overload.
Or maybe the blame is on patients who, despite all the proclaimed efforts to engage them, are still shy to decide on their own health? We consider ourselves professionals when demanding the ban of Nuclear Power stations in favor of a “cleaner and greener” technologies, but suddenly feel ourselves meek submissively accepting the risk of surgical procedures. We obediently swallow medications prescribed according to statistical tests, without asking why the given pill would work exactly for us, and we accept diagnosis and treatments without checking for alternative approaches.
For example, many cardio patients are undergoing expensive bypass surgeries. The bypass procedure is not harmless. The estimations are that following bypass only 75% of patients remain free of cardiac ischemia for five years, dropping to 50% by ten years. Meanwhile there are safer (though more primitive) methods existing for over 50 years for treating angina such as, e.g., External Counterpulsation (ECP) that is completely non-invasive. A computer microprocessor triggers the sequential inflation with compressed air of cuffs that are wrapped around a patient’s calves, thighs and buttocks. As the computer inflates the cuffs, blood is propelled from the lower body back into the heart. This action facilitates venous return of blood into the heart, increasing cardiac output. Does this method work for you? Maybe not, but at least it is worse to check it with your doctor.
So why there is no pressure from us citizens to stimulate medical community to crave for new and perhaps better methods of treatments like it is happening in other industries? To be honest, I do not have an answer, but I think it is time we should feel and behave ourselves less like sheepish patients, but more like citizens and customers of the healthcare system which we are directly or indirectly funding.

The forecast for wearables is still bright. Studies show that one in six (15%) consumers in the United States use smartwatches or fitness bands such as Fitbit, Jawbone, Nike, Apple Watch or Microsoft Band. While around 19 million fitness devices likely to have been sold in US in 2016, the outlook for 2018 reaches 110 million.
Heart rate can now be measured with a device combined with oximeter built into a ring or a watch band; muscle activity can be tracked by an electromyographic sensor embedded into clothing; level of stress is estimated with an electrodermal sensor incorporated into a wristband, and sleep patterns via an accelerometer in a watch. All those gadgets of course are generating numerous self-tracking applications such as food monitoring MyFitnessPal or Zeo sleep analyzer.
Nevertheless, surveys signal some alarming trends. 32% of users stop wearing their tracking devices after six months, and 50% after one year. Many are bored of constantly entering and tracking multiple data with no clear evidence how the process is affecting their health. Without getting tangible functional value from wearing extravagant devices, people are unlikely to change their habitual life style.
Who is using wearable devices?

Curiosity is one of the powerful drivers stimulating people to try new things. 75% of wearables’ users described themselves as “early adopters” of innovative technologies. No wonder that 48% were younger than 35 and 29% reported to earn more than $100.000 annually. So, basically, to become a user of a modern wearable device one should be young, healthy and wealthy. Most of Fitbit, Nike, Runtastic, etc. users are already sport fans accustomed to care about their health. Fancy gadgets are just adding more fun.
Apparently, this is not the prime target group that needs to improve its well-being. But wearables could be a solution for real problems, e.g., long-term chronic condition management or remote care. The technology has a potential to create healthy smart homes where seniors and those suffering from chronic conditions could feel themselves safe and secure. For example, a microanalysis of body movement data can be used to detect early symptoms of Parkinson disease . Such a widely popular game device as Microsoft Kinect equipped with a high resolution camera and infrared sensors is able to grab the slightest, almost invisible facial and thorax movements including tissue vibration to predict sleep apnea or a sudden cardiac arrest. All this is possible but requires a big change on behalf of the user: tolerance to adjust to the devices, diligence in monitoring vital signs.

The change is not easy. Most of those who potentially can benefit from wearables are of 50 and above age, the generation of workaholics, “company best assets” truthfully serving their employers. For years, they have been used to long overtimes, sacrificing their sleep and weekends to finish a crucial report impossible to accomplish in-between daily meetings and conference calls. Will this people be ready to withstand the demand and pressure of social obligations and sacrifice precious moments of their life that can be spent with families and friends for the sake of fitness trainings? After all, years are passing by, and there are still some things to do in this life besides reaching the goal of 5000 -10.000 steps per day.
If they will, then under one condition: wearable gadgets should add a real value to people’s life. Unfortunately, the achieved number of steps and the associated weight loss do not directly help to improve serious health issues such as hypertension, diabetes or cardio failure. On the contrary, several studies have observed that patients with type 2 diabetics who self-monitored their own blood glucose concentration did not benefit from increased glycemic control but rather found their disease more intrusive. Excessive self-quantification along with persistent inability to improve one’s health conditions provoke the feeling of helplessness that may lead to anxiety, frustration or even depression, which, in its turn, can hardly ameliorate symptoms of health disorder such as increased AD, sleep disturbances, irritability, hot flashes and other vasomotor instabilities. A number of trials show no beneficial effect of blood glucose self-monitoring among non-insulin treated patients, while others demonstrate negative outcomes, including elevated levels of depression.
Can we trust wearables?
Getting data is not enough, one should trust information it provides. The reliability and validity of data produced by wearable devices in many cases is questionable. For instance, comparisons between various types of wearables tracking physical activity showed large variations in accuracy between different devices — with error margins scaling from 10% to 24%.
It is relatively easy to count steps, but understanding the correlations between those numbers and more complex indicators such as daily energy expenditures (EE) across many devices is much more difficult. Thus, comparisons between research-graded accelerometers/multi-sensor devices (BodyMedia SenseWear, and ActiGraph GT3X+) and consumer wearables such as Fitbit One, Fitbit Zip, Jawbone UP, Misfit Shine, Nike Fuelband, Striiv Smart Pedometer and Withings Pulse demonstrated a relative consistency in step counts, however correlations in EE were only around 30%.
It is also important what exactly physical parameters wearable sensors are measuring. Take for example sleep trackers. Unlike the professional polysomnography (PSG) equipment that is tracking multiple sleep pattern parameters, e.g., brain wave characteristics (EEG), blood oxygen level, heart rate and rhythm, breathing patterns (how easily or difficult you breathe, how often you stop breathing, pauses in-between inhale and exhale), eye movements, etc., the majority of self-assessing sleep monitoring wrist accelerometers are simply tracking body motions, at best in combination with pulse). But what if a person is having insomnia, but deliberately is trying to lie still? So, in a way we are sacrificing quality for the sake of usability and price.
Time is one of the most precious and vanishing values in our life, especially for those who have real health problems. If people are investing their time to change their habits, preferences and life style they want to get a meaningful return of investment. While wearables help to achieve short-term goals with diets and exercises and, possibly, temporary weight loss, a long-term impact of consumer wearable devices on complex health issues such as hypertension or diabetes is still questionable. But hope is the last one to die. Saying that I am rushing to reach my 10.000 steps goal.
The annual international conference on Wearable Technologies did not impress by innovative discoveries, but rather showed the meaningful utilization of the existing ones.
Many of the demonstrated products such as smart watches, wearable garments, smart caps or badges were based on already existing technologies, e.g., measurement or registration of the following physical phenomena: light signals (LED), heat conduction, galvanic skin response (variations of electrical conductivity of the skin), local pressure changes, fluid velocity distribution, chemical detection of substances or using electronic sensors of small electric currents.
However, there was a definite step forward. Contrary to the first wave of digital gadgets mostly preoccupied with fitness and wellness parameters such as heart rate, number of steps and burned calories, the demonstrated at the conference devices were primarily focused on collecting data relevant specifically to health.
Thus, Xsensio presented its “Lab-on–SkinTM” device developed at the Swiss Institute of Technology. Miniaturized nanotech sensors are analyzing chemical biomarkers such as electrolytes, proteins, molecular or bacteria right at the surface of the skin for real time early diagnostics.
CSEM , another Swiss company, in cooperation with Smartwatch is designing a spectrum of bands and watches with intelligent chips that will allow users to measure blood pressure, something that developers were yearning to achieve for years.
Most of commercially available blood pressure monitors and respective online applications are standardized for the “average person”. Thus, the allegedly “correct” numbers for systolic and diastolic are, e.g., 120/130 vs. 70/80 are stipulated irrespective of a person’s age, gender or physical condition. A CSEM device is linked to an application to calculate individual’s weight, age, gender and height adjusting the “correct numbers” to individual health conditions thus helping people to develop their own personal blood pressure protocols and avoid unnecessary panic or medication consumption.

Smart clothing is apparently the rising trend of the personalized healthcare. The wardrobe of wearable garments such as HealthWatch or Niturit ECG monitors is being enriched by new fashions. Bonbouton , smart T-shirts designed by a US start up, is using graphene sensors embedded in the normal textile fabric. Graphene has a strong potential for wearable sensors due to its unique capacities to ensure both thermal and electric conductivity as well as high breakage strength. The material can be used in the standard devices collecting multiple vital sings from temperature variations, breathing rate, pulse, ECG, and beyond that can be applied to the vast spectrum of healthcare objectives.

AiQ smart clothing is another attempt to merge electronics with fashionable textile.Based in Taiwan, the company is designing the variety of comfortable garments such as TouchMan gloves made of conductive yarn that is woven into the glove fingertips allowing to touch panel devices with accuracy and precision, without the inconvenience of removing your gloves; ThermoMan electronic thermo garment tracks the local body temperature. After grasping the body temperature the garment is releasing the respective amount of heat to keep its user warm; ShieldMan, an anti-electromagnetic (EM) radiation textile is designed for young mothers to protect the fetus from harmful EM radiation impact.
It is impressive how relatively small startups are successfully addressing the biggest worldwide problems such as child mortality. Nearly three million newborns die every year in the developing world due to acquired infections, injuries, birth defects or pregnancy complications. 80% of such deaths could be prevented, should medical help have been provided on time. Unfortunately, these countries are still chronically lacking professional medical resources.
Neopenda, a US engineering team of young enthusiasts, addressed the challenge by creating a small wearable device that remotely monitors vital signs of critically ill newborns. A low powered multiparameter sensor arrays are measuring pulse, respiratory rate, peripheral blood oxygen saturation and temperature. The system can be installed at the newborn’s home alerting physicians nearby or those in a hospital in low resourced areas.

Unlike their laboratory created predecessors, many wearable products demonstrated at the conference are already commercially available. SmartCap, developed by the Australian company, has now found its practical utilization among machine workers.

Tiny sensors embedded in the typical baseball cap are capturing electrical activity of the brain estimating the level of fatigue of its user. Early warnings alarm when exactly the worker should interrupt the activities to take some rest. The system is much favored by long distance drivers of heavy tracks, mining industry workers or by aviation pilots. Maybe soon office workers will be wearing such caps to estimate the best productive time for their customer meetings or politicians to vote on important public regulations.
Printed electronics such as wearable patches or bandages is another rapidly developing technology that helps to unobtrusively monitor health parameters such as local temperature, skin humidity or ECG identifying health issues on a very early stage.

Thus, professor Matti Mäntysalo from the University of Tampere in Finland is working on a bandage with electrodes printed on stretchable bandage material that measures the heart’s electrical activity transmitting signals to the cell phone.
Not only wearable devices are now actively searching for commercial utilization, they are now capable of generating new businesses and jobs. Thus, the first wave of wearable designers was practically covering the whole production cycle: from idea, design up to the finished product. Now developers tend to delegate parts of industrious procedures to professional companies. Thus, Convestro, a world-leading supplier of high-tech polymer materials, is specializing in production of adhesive tapes, badges, patches and film coating for embedded sensors incorporated in wearable devices. Since sterility, elasticity, sustainability to external factors such as pressure, heat or rupture are the top requirements for medically used materials, it is cheaper and safer to delegate the business to professionals.
The general impression is that the industry in gaining maturity. The developers are moving away from “cool technologies” to “proven and accurate” commercial products that will be able to collect and analyze meaningful data to provide healthcare industry and citizens with deep insight on their health. Who knows, maybe soon we will finally be able to try a smart dress with a fancy sensor hat in a fashionable boutique or an elegant smart bracelet in a jewelry shop.
Swallowing antibiotics prescribed by my doctor to treat bronchitis, I imagined how nice it could be if my doctor noticed the effect immediately. I may cut on antibiotics in case fever drops or, on the contrary, take more appropriate measures in case it jumps up. I should not wait in complete uncertainty for the next visit .
Working in IT my first thought would be to use some fancy application. But as a patient with a fever all I need is help. I needed services vs. just pumping my application with data nobody cares about except myself.
We are feeding our mHealth apps with multiple isolated data such as temperature, blood pressure or even ECG, but without constructive follow-ups this is just a trash that provokes more questions than constructive actions. Is it not the cause of consumers’ disillusionment in mHealth apps?
According to the results of Research2Guidance mHealth App Developer Economics 2016 study, the demand for mHealth applications is decreasing, while their offer is increasing. A total of 3.2B downloads are expected in 2016 with 259,000 mHealth apps listed on major app stores. A total increase of +7% compared to 2015 which is a significant drop down compared to 35% and 36% mHealth application growth in 2014 and 2013.

Can such a trend be reversed?
Allow Hospital Information Systems to collaborate with patients.
The Hospital Information Systems (HIS) were initially focused on supporting inner hospital procedures such as access to Labs and Pharma, clinical data repositories (CDR), nursing/clinical documentation, computerizing Practitioner Order Entries (CPOE) thus creating a collaboration environment within medical staff. The trend is still sustainable. While consumers are more ready to accept mHealth applications to monitor Health conditions and share it with their doctors, studies show that medical community is still more conservative in enrolling patients’ data into the care process.
Thus 77% of US consumers, according to RockHeal+t study, are eager to share their health information to get a better care from their doctor. Medical staff, on the contrary, continue seeing more value in physician-to-physician and nurse-to-physician communications. This was highlighted by 78% of medical staff according to Spok’s annual Mobility in Healthcare Survey.
Of course, there is much less risk in pumping a standalone application with patients’ health data vs. integrating such data into medical procedures. The validity of information, the reliability of devices that generated data as well as the trustworthiness of applications is still much to be desired. But the value of such information is lower: if mHealth apps will not entail adequate health services the overall mHealth disillusionment will grow.
Advanced analytics in consumer apps.
Most of consumers mHealth apps are primitive data repositories still waiting for analytical engines to process floods of confusing data. They will collect your blood pressure or glucose level for months and years. Alas, those regularly collected and averaged observations still do not suggest how to improve personal health results. The majority of today’s consumer health apps are unable to interpret relationships between the vast spectrum of personal health data in order to finally build a full picture of the health puzzle – to improve either an individual’s daily habits or health treatment.
No surprise that after several months of diligently collecting it, the enthusiasm is fading and users stop downloading the apps. A study from the Journal of Medical Internet Research (JMIR) shows that even patients who do see value in smartphone and tablet apps nevertheless stop engaging with the devices within 6 months. More than forty percent said that tracking and monitoring apps required too much time to input necessary data, while a similar number simply said that their interest faded over time.
Adoption of wearable sensor technologies in care procedures.
Wearable devices enabling consumers to “ quantify self” are originating floods of mHealth apps. The Global Wearable Sensors Market according to Mordor Intelligence Survey will grow from $3.75 billion in 2014 to $14.75 billion by 2020, at a projected CAGR of 25.7% “Smart Pills Technologies Market (2012-2017)”; the report forecasts the global smart pills market to reach $965 million by the year 2017 whereas Gartner expects shipments in the smart garment category to jump from 0.1 million units in 2014 to 26 million units in 2016.

Devices and apps such as AliveCor Kardia Mobile that provides one channel ECG results in 30 secs with the help of a sensor attached to the mobile phone; a t-shirt developed by the University of Aveiro in Portugal and the Israeli “Moked Enosh” that records the heart activity over a number of hours transmitting it via a smart phone from a patient to a cardiologist; the smart patch created by researchers of University of Illinois, Urbana-Champaign, that can be stuck to the skin for continuous EMG and EEG monitoring – all those technologies will generate thousands of mHealth applications and data. Will hospital information systems be ready to encompass data from all those devices for early diagnostics and personalized therapy? Currently only 8% of US hospitals covered by Spok survey supported wearables in their organizations.
Adequate infrastructure to support mHealth application services.
An adequate infrastructure including secure data storage, sharing and analysis is still one of the major blockers preventing hospitals from the efficient use of mHealth applications. While most of mHealth app developers already use the existing vendor platforms such as Apple HealthKit (69%), Google Fit (44%) or Samsung S-Health (18%), many hospitals are still locked within their own world. The absence of a secure infrastructure allowing the hospital staff to integrate patient’s experience across care was identified by 54% out of 550+ US hospitals.
Conclusion: As a person I would not object to becoming a guinea pig for new devices and applications and change my behavior to manage my health. But I would expect the adequate behavior change on behalf of my physicians. Me – to track my blood pressure, BMI, heart rate, etc. to better handle my own health, my physician – to provide better diagnostics and personalized therapy. It will be critical over the next coming years to turn mHealth consumers’ apps into patient centric services, in particular, by integrating them into healthcare processes and systems.
East oriental medicine such as Traditional Chinese Medicine (TCM), Japanese Kampo or Indian Ayurveda often provokes skepticism in the professional medical environment. And for the right reason: despite thousands of years of empirical observations, oriental practices are still lacking scientific evidence based on verified experiments. Moreover, it is hard to comprehend within the frame of the European thesaurus the TCM concepts of Qi as life gathering or the Ayurveda notions of Vita, Pitta and Kapha. Can anyone intelligibly explain the meaning of Vita and that it is composed of air and space? Or the concept of Shen-nong, in particular implying the lungs’ relation to metal?
In general, can the methods of modern science and technology be applied to verify such ancient concepts?
Body as a Machine vs. Garden.
The crucial distinctions between European and traditional oriental health practices is the notion of Health vs. Medicine. Although “health” and “medicine” are commonly used interchangeably in various contexts, there is a decisive difference between them. European medicine was adhering to the presumption that diseases mainly arise from erroneous behavior or unreliable functioning of individual body organs, partly genetically determined. Hence the therapy was historically focused on deficiencies of separate organs manifested through physiological features, e.g., skin color, gait, BMI (body mass index), pulse rate, blood pressure, etc., with the attempt to bring it back to the “normal conditions” often by means of radical interventions.
This approach is reflected in the overall structure of contemporarily healthcare system split along various disciplines: oncology, genecology, gastroenterology, cardiology… The human body resembled a machine with a set of mechanical spare parts. When some are damaged, they must be fixed or replaced. A crucial principle underlying all complex systems (and human organism is one of the most complex systems) that sum of the parts does not constitute the whole was practically neglected.
Contrary to that, oriental physicians believed that the body is an organic whole where all its parts are interconnected and can pathologically influence each other. There is no such thing as a partial health. People feel themselves healthy as long as their organisms are capable to maintain stability under an influx of real-life influences such as stress, psychic overload, microorganisms, fungi, allergens, parasites, etc. The possibility of a disease may not spring from the failure of a distinct body part (organ), although it can be manifested as such, but can be the property of the whole organism (e.g., with elderly people who may feel themselves unhealthy although all their physical parameters remain within the norm).
Ancient oriental physicians perceived body as a landscape, a functional macrosystem constantly interacting with the environment. If a river stream is contaminated, it may not lead to the pollution of the whole freshwater, but if the ecological balance is distorted, the river may be turn into a swamp.
The latest achievements in nanotechnology, the design of miniature nanosensors capable of tracking multiple physiological parameters of the human body can bring modern medicine closer to the ideas of holistic health. There are some good examples such as smart tattoos designed by the University of Illinois. Such a tattoo represents an implantable skin mesh of computer fibres thinner than a human hair that can monitor and quantify human body’s inner processes. Similar research in the area of electronic skin is carried be the team of experts from Northwestern University’s medical school or in Chicago together with the University of Tokyo.
Miniaturization of devices leads to getting smaller and smaller down to the size of dust. The researches in UC Berkeley, MIT and the University of California, Los Angeles, are preoccupied with Smart Dust , the arrays of full computers with antennas, each much smaller than a grain of sand that can organise themselves inside the body into as-needed networks. Though still in the initial stage, such technologies can allow a pervasive monitoring of the individual health status.
Body as a regulated self.
The TCM Shen-nong teaches that the body is an organic whole where each of its 5 elements (heart, liver, spleen, lung, kidney) complements each other to perform life activity. The 5 elements are connected via so-called meridians, this distribution network of Qi. The disruption of connections provokes disharmony and disease.
To help the body to regain its balance a physician needs to constantly tune the therapy to the body response. But to spot and understand physiological feedbacks is more Art than Science.
Modern nanosensors can not only collect biofeedbacks, but react on them, exerting control over complex chemical reactions and metabolical processes within the organism.
In case of acquired diabetes (DM-2), one of the examples of the body metabolic distortions, the beta cells located in pancreas are either damaged or fail to produce the required amount of insulin.
To keep the glucose levels under control, the researchers at the University of North Carolina and NC State created a smart patch. The patch is coated with culturally produced human beta cells that are responsible for monitoring the excess of sugar in the bloodstream. Tiny microneedles are attached containing the glucose-sensing enzyme. Poked into capillaries, the enzyme spots the sugar increase and communicates this message back to the beta cells. The mechanism is fixed and beta cells regain their functions.
4 pillars of TCM Diagnostics.
Looking/smelling, listening, asking and pulse palpation are the 4 pillars of TCM diagnostics. Body fluids exerted in urine or sweat perform an important metabolic function of “cleaning the body” from toxins and wastes. TCM doctors paid a lot of attention to sniffing even tasting urine to diagnose Kidney Exhaustion Qi (Xu) or Stagnant Bladder Qi (Excess). Modern technologies allow to run such tests in a more elegant way. Moreover, it may become part of the daily routine. HealBe, a company specialized in wearable devices and wellness applications, is raising “crowd funding” to create device that will quantify sugar level in the urine. GlucosAlarm can be simply installed in a toilet. Sensors will be measuring sugar, but also some proteins, e.g., albumin as well as ketones, pH, etc. to detect a wide range of disorders such as urinary tract infection, kidney diseases and many others.
Smell exhaled through breathing is another important parameter of TCM diagnostics. It may signal Lung Qi and Lung Yan excess or deficiencies that may cause, e.g., lung cancer or gastrological disorders.
The new wave of breath analyzer technologies, such as Na-Nose designed by the Israel Institute of Technology researchers under the leadership of Prof. Hossam Haick can verify empirical sniffing with objective analysis. Coated with tiny nanowires Na-Nose sensors are reacting on chemical compounds exhaled with the breath measuring the concentration of cancer biomarkers contained in them. The technology is successfully applied to diagnose lung cancer or various types of gastrological disorders.
The vitality of Qi and immunotherapy.
TCM and Ayurveda physicians believed that vitality is achieved via activation of the vital energy of Qi and Yin/Yang harmonious interplay, the approach that resonates with the modern concept of immunotherapy.” Contrary to such methods as chemotherapy that suppresses not only the tumor cells, but the whole immune system, the immunotherapy uses “body’s own immune system to help fight cancer”. For example, such medications as Keytruda (pembrolizumab) or Iskador/Mistletoe (medication derived from semi-parasitic plant that grows on oaks and other trees in Europe and Asia) are already used to combat melanoma or lung cancer by activating the immune system.
But the effective antitumor immunity requires a clear understanding of how the immune system senses and responds to threats, including pathogens and tumors.
The researchers from Tel Aviv University under supervision of Prof. Dan Peer noticed that Mantle Cell Lymphoma MCL is associated with the intensified activity of a certain gene, namely the gene CCND1. When over-expressed, the CCND1 gene produces too much of a Cyclin D1 protein, sometimes 3,000 – 15,000 times too many. To reduce and regulate protein production the scientists have invented the CCND1 blocker: the synthetic strand of RNA molecules (siRNA). By targeting RNA molecules that convey genetic information from the DNA to the ribosomes, the inner-cell structures where new protein chain are assembled (translated) from amino acids, siRNA disables its ability to express a specific gene. To deliver siRNA precisely to CCMD1 gene, the former is loaded into the lipid-based nanoparticles (LNPs) coated with antibodies. Scientists believe that such method could be applied not only for MCL but also for other malicious forms of cancer.
Conclusion.
Traditional oriental practices gained over 5000 years of empirical observation of human organism. Unfortunately, the absence of scientific evidence often gave way to all sorts of charlatans, quackery and quasihealers. European medicine, although younger, has some outspoken advantages. Driven by industrial and scientific developments it has enriched healthcare with the discoveries of genomics and applied physics (e.g., nanotechnology, microprocessors, microwave and nuclear technology, signal and image processing, etc.). The rapid expansion of quantum sensors designed to convert the body physiological characteristics such as pulse rate, blood pressure, ECG (electrocardiogram), EEG (electroencephalogram), HEG (hemoencephalogram), REG (rheoencephalogram), PPG (photoplethysmogram), ENG (electronystagmogram) and EMG (electromyogram) signals, local thermal (infrared) emission, skin wetness, etc. into sequences of electric pulses and further into digital signals as well as implanted nano and biosensors able to track chemical reactions inside the body will allow to test oriental concepts with objective experiments. If such experiments are successful, the oriental therapy and the European medicine (“the school medicine”) can be transformed into a single health science.
One of the fundamental transformations of the European healthcare system is a changing position of a patient vs. a physician. A physician, traditionally perceived as a Demiurge able to decide on life and death due to the unique knowledge of Ars Medica he possesses, is giving space to a patient, whose previous role was to submissively tolerate procedures imposed on him. Hence the word “patient”, not “person”, adopted in medical environment.
Consumer-oriented technologies such as smart phones, tablets, etc. intrinsically support the concept of a “patient centric care” which means granting more decision power to people through the ability to access personal health data, search for an appropriate doctor or verify their diagnoses. By pushing their gadgets with applications into the environment previously dominated exclusively by professional medical devices, consumers are gradually becoming one of the key drivers of the whole healthcare market making it more patient oriented and human. But there are several blockers on the way.
Blocker 1. Patients’ disengagement of the Health Information System (HIS) design.
 By influencing business processes HIS has a unique ability to guide and drive the user’s business behavior. Consequently, if HIS does not stimulate users to behave differently, they will run their business in the old way. Thus, according to American Hospital Association survey 2014, 80% of provider organizations have some type of basic EHR (Electronic Health Records) in place, but only about 35% had “comprehensive” systems rather than merely the ability to share clinical notes.
By influencing business processes HIS has a unique ability to guide and drive the user’s business behavior. Consequently, if HIS does not stimulate users to behave differently, they will run their business in the old way. Thus, according to American Hospital Association survey 2014, 80% of provider organizations have some type of basic EHR (Electronic Health Records) in place, but only about 35% had “comprehensive” systems rather than merely the ability to share clinical notes.
HIMSS EMR (Electronical Medical Records) maturity adoption model shows that only 217 hospitals (around 15 percent) of the total 5,627 US hospitals have achieved the EMR 7th stage thus, according to the stage requirements, being able to share health records with their patients.
Physicians are often part of the development teams as testers or consultants. If a doctor does not get what she/he needs with more than one or two clicks the system is not worth working with. Patients, on the contrary, have much more limited representation in the development process. But after all, who is the one who will ultimately endure the outcome of medical procedures? Why not putting patients on board of the software design teams to enrich the system from the very start with patient oriented services such as homecare or remote monitoring.
Unfortunately, so far efforts to create Personal Health Record Systems (PHR) destined to capture individual’s preferences or complains are running in parallel to HIS or EHR developments. A future integration of such systems could be a nightmare. Not only interoperability and security pose great challenges, but most of the physicians rightfully do not trust the data received from external sources. After all, how those data were obtained? For example, was a patient sitting, standing or exercising while her/his blood pressure was taken? How reliable was the device that was used?
There are some good examples of clinics that start enriching their EHR and HIS with patients’ PHR. For example, Mayo Clinic personal health information tool is offered to patients as services enabling them to view the “results and records as fast as your clinician does”. Medical Archive – a Personal Health Record application – designed by a group of enthusiasts from the Moscow Hematology Institute helps patients to review treatment procedures discussing, together with clinicians, the latest lab test results for the sake of the overall outcome improvements. Unfortunately, such practices are not yet wide spread.
If health information systems are to drive clinicians towards new behavior and patient relationships, the approach should be embedded in HIS from a very beginning rather than piecewise mending various parts of EHR, EMR and PHR later.
Blocker 2. Incompatibility of traditional business processes and Digital Era.

One cannot drive a Harley Davidson the same way one rides a bicycle. The present care delivery model does not fit the Digital Era goal of offering accessible health services to many anytime anywhere. Doctors will hesitate to provide online consultancy if their compensation is based on a number of face-to-face visits (model existing, e.g., in Germany). Similarly, a US physician whose licenses are tied to Nebraska would not be able to support patients in Alabama.
The long-awaited personalization of care promised by the Internet of Things or by personal genomic studies clashes with the traditional insurance compensation based on “one size fits all” practice.
Hospitals and physicians who are receiving premiums from insurances for each operation performed, even the unnecessary ones, are hardly an example of a patient-safety approach. Thus, the German Health Insurance AOK 2014 report provoked indignation among both physicians and hospitals when it revealed that 19.000 preventable hospital deaths in the country were annually happening as a result of operations that could have been avoided. For a comparison: car accidents took away the same year 3.290 lives.
ICT could catalyze new methods and positive behavior shifts in healthcare, but if it supports fruitless business process, it can be a guardian of stagnation.
Blocker 3. “Digital fears”.

True, current EHR systems are still much to be desired in terms of their friendly look and feel. But let us also not underestimate another reason: a deep belief stemmed from the long history of medicine that a doctor belongs to the sacred guild with an untouchable authority. Technology brings transparency, including the disclosure of medical errors that makes the authority relied exclusively on belonging to a professional group vulnerable.
Despite all technological innovations, it is often a human factor that decides on what “to be or not to be”. How often have we heard from physicians that EHRs slow them down by forcing to tangle with complex interfaces instead of spending time with a patient? According to a American Medical Association and the American College of Physicians’ American EHR division., about 34 percent of physicians said they were satisfied or very satisfied with their EHR in 2014 whereas 72 percent believed their EHR made it difficult to very difficult to decrease their workload.
I was once visiting the newly renovated hospital in Munich with SAP Healthcare system installed across its departments. To my surprise, the Intensive Care Unit (ICU) staff was not able to access records of a patient who was brought to them from the cardiology department. Nor cardiologists were able to access records of the same patient who had been previously treated by neurologists. The clarification was astonishingly simple: if a clinician uses data provided by another clinician, he should be prepared to share information about his/her own patients. Something, as I was explained, many physicians do not want due to the fear of transparency. Thus the “continuity of care” could simply bump and break against the human desire to protect one’s territory.
Contrary to physicians, the majority of patients have a different attitude to EHR. A survey launched by Nuance found that 97 percent of patients are comfortable when their physicians are using EHR. Moreover, according to ReferralMD, 54% of patients are very comfortable with their health providers seeking advice outside, even from online communities, to better treat their conditions. Such activities in no way undermine patients respect towards their physicians.
The information technology can support and drive positive transformation in healthcare. But it is not a magic. It is just a tool that could be used to get a better insight into clinical history, provide better diagnostics and successful treatment. It depends in whose hands the tool is and whose interests it protects. Ideally, it should be in the possession of both patients and medical professionals united by the common goal: to find a right treatment for the right person.
Numerous devices are coming out stimulating people to control their vital signs, workloads, steps, sleep measuring slightest deviations from health equilibrium. Twenty percent of Americans are owning now a wearable medical device. 56% of those believe that by monitoring their vital signs they will increase life expectancy at least by, in average, 10 years. According to a MarketResearch.com report, the Internet of Health (IoH) market segment is poised to hit $117 billion by 2020.
Starting with sport and wellness smart bands are building a bridge between consumers and professional medicine, promising to be more than just activity trackers. Dartmouth Hitchcock, e.g., is using Microsoft Band in combination with Cortana intelligent assistant to help physicians and nurses monitoring patients remotely.
Medical professionals are setting up their companies to step into the lucrative consumer markets. Kardia Band, the first medical-grade EKG band equipped with ultrasound sensor unveiled by AliveCor, will tell you in 30 seconds if your heart works normally or you are having a cardio fibrillation. Simply press you thumb to the watch screen. Similarly, large corporations are hurrying to promote their products. Thus Phillips has revealed its optical sensor embedded into consumer’s hand band to accurately track blood volume variations recalculated into the heart rate.
Sensors can capture not only your physical, but also emotional parameters. Zensorium watch-like device claims to predict, for $129, if the wearer is distressed, excited or calm by measuring the change in intervals between heartbeats. The technology can step further to manipulate your moods. Thync, a company founded by Harvard neuroscientists, developed a sensor that is instructing nerves on the head and neck to act on the brain adrenaline system. Attached to the temple, it changes the wearer’s mental state able to energize or to calm a user down.
 Even the gaming industry is hopping on the health trend. Microsoft Kinect2.0 is measuring heart rate remotely by assessing the amount of color intensity radiated by the face during heart contractions. You can peacefully exercise at home while watching the workload’s effects on your heart conditions.
Even the gaming industry is hopping on the health trend. Microsoft Kinect2.0 is measuring heart rate remotely by assessing the amount of color intensity radiated by the face during heart contractions. You can peacefully exercise at home while watching the workload’s effects on your heart conditions.
More and more companies are realizing that health of their human resources is an asset and the expensive one. Thus according to Mercer L.L.C. the group health care costs rose to an average of $11,635 per employee in 2015.
It would be natural to assume that healthy, sporty, stress tolerant employees can work harder for the company generating more revenue, while significantly savings on healthcare costs. The assumption forcing corporations to continuously invest in employees’ Health and Wellness programs. And so they do. Tamarac, Florida-based City Furniture Inc., which saw a 3.5% increase in group health costs per year, has produced a health reimbursement arrangement plan. Now 80% of its 1,300 employees are enrolled in the program.
British Petroleum (BP) provides its employees with 16,000 FitBit devices adjusting its employees’ health care premiums depending on how much physical activity their wearables monitor. This allowed the company to drop healthcare costs below the national growth level.
The Return on Investments (ROI) is of course expected. The exchange could be your health data consequently calculated into revenue. CVS Pharmacy, e.g., demands that every one of the 200,000 employees who use its health plan provides certain information about weight, glucose levels, and body fat. Although CVS calls its plan “voluntary,” covered workers who refuse to provide this information must pay a fine of $50 per month.
Soon the devices will be able to “quantify” you from top to bottom. Internet of Health is offering an Employer an unprecedented chance to collect enormous amount of data about employees to assess their staff within a short period of time.
Just imagine your friendly HR is presenting you with an attractive fitness device as a Christmas present. You may think it is a nice gift, but there could be a pragmatic plan beneath the corporate Health and Wellness benefits.
What if your HR suddenly learns that despite all the programs you have been so generously offered your blood pressure is still high and the sugar level is not decreasing? Is it really hard to imagine that upon learning that the efficiency of your sleep is below 50% after attending the company meeting or 1:1 discussion with your boss, a long awaited promotion will suddenly be granted to your more “stress tolerant” colleague?
Of course generating data from employee’s devices and using them for discrimination due to disability, illness or ages is illegal. On top of that the Employer should be getting non-identified group data. But is it so difficult to identify a person among the group of, e.g., 5 people? After all let us not forget that all wearable gadgets and devices are normally provided by the company and thus are still part of its own property. So why not the data collected from those devices? Are the security rules strict enough in regard to Wellness programs?
Last year a City of Houston has introduced a wellness program to all government employees. To their regret, the participants found later that the security and privacy were absolutely not taken for granted and “review of privacy policies shows that many wellness vendors adopt policies allowing them to share identifiable data with unidentified “third parties” and “agents” working to improve employee health.”
Of course no Human Resource (HR) in his right mind will venture to get rid of an employee on the ground of poor health. Much more elegant and efficient pretexts such as “lack of leadership skills”, “poor communication” and ultimately “insufficient performance” are elaborated to disguise the intention.
Many companies are trying to get rid of their senior employees under such impartial umbrellas. It is a company “best kept secret” that people above 50 should be on the “to go list” in search of “new opportunities”. It should not come as a surprise that people who are laid off by the company due to “restructuring”, “transformation” or “job elimination” are predominantly over 50. This is exactly the group that is approaching the brim where health may start giving up and health premiums should be increased. Is it perhaps the reason why those people are trying to avoid the enrollment on the fitness programs? According to the studies only 7% seniors are owning a fitness device.
Why not to take two healthy youngsters aged about 25 vs. a single one over 50 who is with extensive experience, but also potential health issues? As one of my colleagues once savagely said: “We need fresh blood!.” I almost heard her phosphorescent white teeth clutching.
Until the complete privacy and voluntariness of the health data collected by wearables under Health and Wellness programs are not guaranteed there is a risk that these data can be misused by employers to discriminate seniors, less healthy, and more vulnerable.
Meanwhile, I have learned that a large company nearby is offering its employees a free medical screening covering multiple areas: blood pressure, liver, heart and kidney functionalities. Are you fit enough to work? Watch out.









 Human senses initially emerged as a survival tool were a valuable clue for ancient physicians to spot the disease. While examining a patient a doctor would carefully touch his limbs, smell his breath, listen to minute body sounds and even taste his urine thus checking the human body without violating its natural functioning nor demolishing natural conditions. Just like animals who are identifying sick species by sniffing.
Human senses initially emerged as a survival tool were a valuable clue for ancient physicians to spot the disease. While examining a patient a doctor would carefully touch his limbs, smell his breath, listen to minute body sounds and even taste his urine thus checking the human body without violating its natural functioning nor demolishing natural conditions. Just like animals who are identifying sick species by sniffing.






Recent Comments